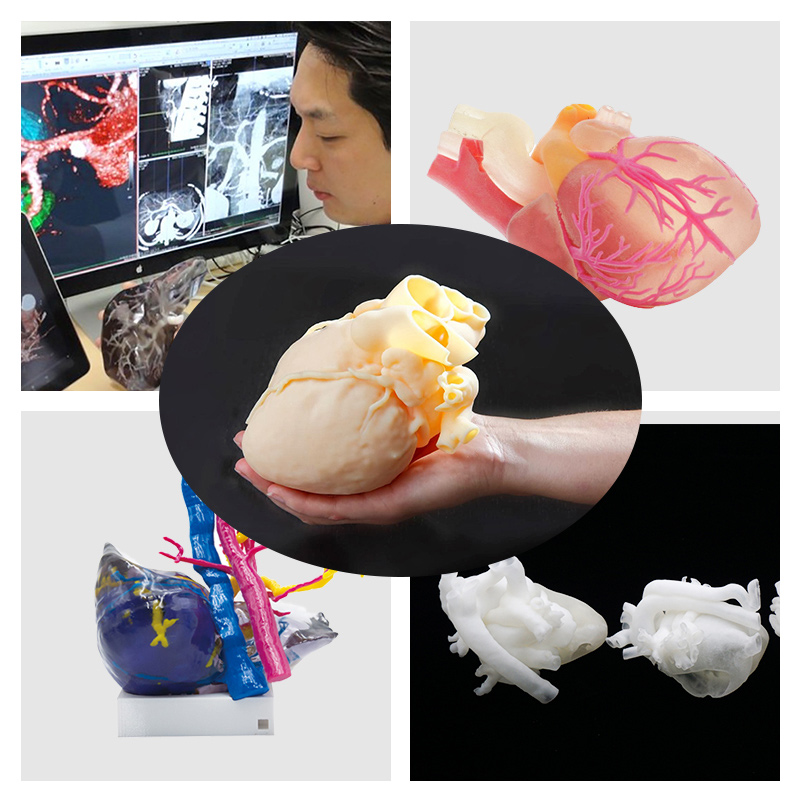
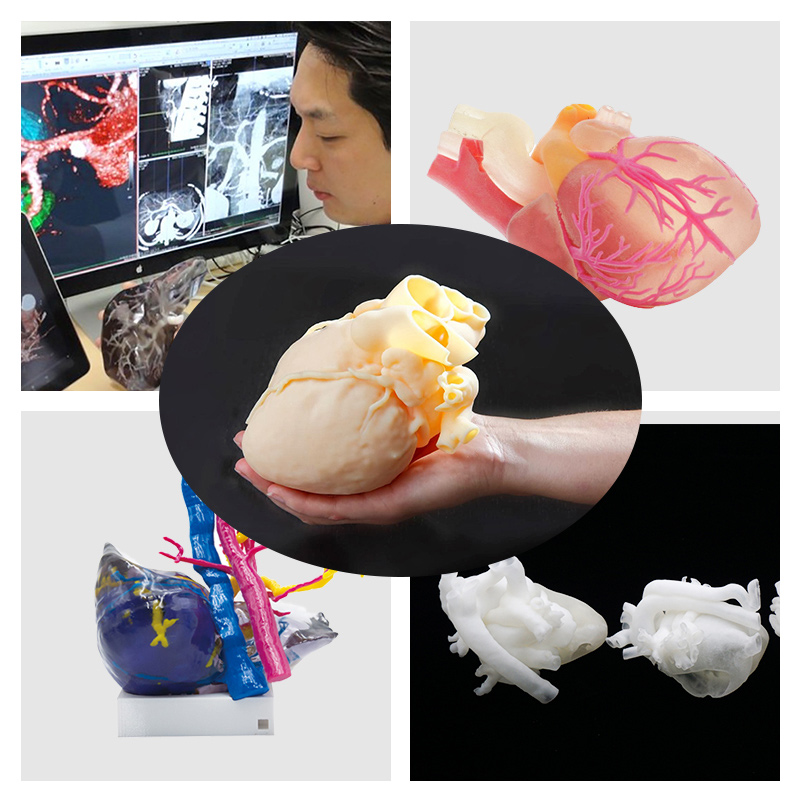
1.Surgical planning and pre-procedural simulation
To attain the best surgical outcomes, cardiac surgeons need to operate efficiently and obtain the best possible surgical result on their first attempt. This requires a keen understanding of complex three-dimensional anatomy, a high level of technical skill, and the ability to make critical decisions in a short amount of time. Each of these factors are enhanced by 3D printing.
When printed in flexible and compliant materials, surgeons can cut, suture and engraft patches, conduits, and essentially perform a simulated surgery before stepping into the operating room. In so doing, surgeons effectively get a “practice swing” before performing the actual surgery. This type of precise pre-surgical planning potentially offers several benefits:
a.reductions in procedure time, which has been linked to improved surgical outcomes.
b.planning for contingencies (Plan A, Plan B, etc) and “bailout” strategies
c.Fewer residual lesions and decreased re-intervention rate
d.Shorter post-operative hospital stay
Given the relatively recent growth of cardiac 3D printing to date there have been no long-term studies to date confirming the potential benefits above. However the clinical utilization is growing, and several papers have reported promising applications of the technology1-8. In addition, early data from the otolaryngology experience is showing reductions in procedure time9-10.
2.Trainee Education
There is an often quoted idiom in medical education: “See one, Do one, Teach one.” This refers to a model of medical training that has persisted as long as the medical profession itself; an apprenticeship model whereby medical trainees learn from the observation and teachings of more experienced clinicians. In the method, teaching is both didactic and experiential, essentially learning through experience on live cases. Our greatest surgeons have trained in this method, and over time they have accumulated a high degree of skill after performing large numbers of cases and committing thousands of hours of practice. At the same time, further examination of this model of medical education makes plain some of it’s drawbacks:
it is highly dependent on the availability of teaching cases – both the quantity of cases and wide variety of complexity required to provide a solid training experience
variability of teaching skill and experience of the educator
learning via practice on actual patients
The last point is particularly noteworthy; it is an inescapable reality of the current medical system, which has overall worked well for generations, though not particularly comforting to patients or their families.
3D printing technologies provide solutions that enhance trainee education to overcome some of the limitations above5. 3D printed models that represent the spectrum of complex cardiovascular abnormalities can be made to for trainees to perform difficult procedures, limited only by their access to the technology. This helps transition from solely an apprenticeship model to a “simulator-based” learning model that have already made other industries safer. As an example, consider the airline industry and training with flight simulators. With 3D printed models we can now provide the next generation of trainees the “1000 hours” (or more) of practice they need performing complex procedures. This new approach augments current education methods and standardizes the ways in which future heart surgeons are trained, hopefully producing surgeons who are better prepared to operate on live patients.
3.Patient and Family Counseling
One of the bedrocks of the practice of medicine is the cultivation and practice of empathy. Empathy is what allows us to put ourselves in our patient’s shoes and imagine their medical experience from their perspectives. It is what helps us connect with the families we serve and ultimately work as a team to tackle medical problems. To that end I invite you to engage in this thought exercise: imagine being a patient, or the parent of a young child, who is learning a complex diagnosis for the first time. Then imagine having to make difficult and complicated decisions regarding this diagnosis, which may involve high-risk surgery. These are the types of situations our patients and families face on a daily basis, and the process of patient and family counseling is fraught with challenges. Some of these challenges have to do with the complexity of the disease, which may interfere with the patient’s ability to make informed decisions about medical or surgical options. For cardiac cases, 3D printed models allow the patient to hold a replica of their own heart while his/her physician goes over their diagnosis, treatment options and the planned procedure. Just as it was for experienced surgeons and trainees, 3D models offers patient a higher level of understanding of their own anatomy, hopefully enhancing the informed consent process, and helping patients and families make better decisions11-12.
4.Future Directions & Transformative Partnerships
While cardiac applications of 3D printing have advanced far in the past decade, the next few years promise to be even more exciting. 3D printing will help push the envelope of personalized medicine, opening up possibilities that were simply unavailable in the past without this technology. One example is cardiac bioprinting, which will allow the engraftment of patient-matched 3D printed cardiac structures (valves, vessels, myocardium, etc)13-14. Other advanced applications include 3D printing for functional 3D modeling, which allows physicians to integrate physiology into 3D models and predict the outcomes of surgeries. Finally, it is very likely that 3D printing using biocompatible materials will be applied to develop the next generation of cardiac implants and devices. 3D printed implants are now routinely used in non-cardiac specialties (ex: orthopaedics, craniofacial, dentistry), and the technology is ready for adoption for cardiac applications. These advanced implants will overcome the limitations of currently available products and further improve surgical outcomes.